Abstract
Background: Allo-SCT is the only curative option for patients with high risk and relapsed/refractory T-cell malignancies. Even among allo-SCT recipients, survival is less than 50% and relapse rates are 55-60%. We developed a clinical trial to decrease relapse after allo-SCT for these patients using romidepsin (rom), a histone deacetylase inhibitor approved for the treatment of relapsed T-cell lymphomas. Based on pre-clinical data demonstrating enhanced and synergistic cell killing with the addition of rom to busulfan (Bu) and fludarabine (Flu) in malignant T-cells, we created a novel transplant regimen (BuFluRom). We hypothesized this regimen, coupled with maintenance rom (m-rom), would enhance malignant T-cell killing, eradicate MRD at transplant, decrease relapse, and stimulate the GVL effect by stimulating NK-cells. Here we present results of this clinical trial, with correlative data evaluating NK-cytotoxicity. This is the first trial designed specifically to treat T-cell malignancies with allo-SCT. (NCT02512497)
Methods:
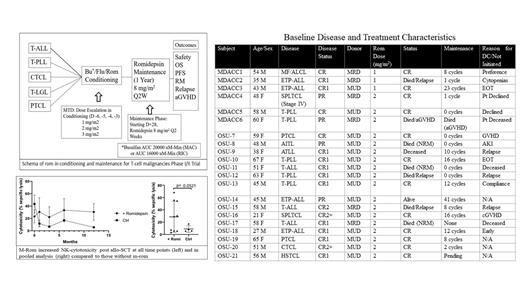
This is a phase I/II clinical trial. Eligible patients had: a diagnosis of T-cell leukemia (including T-acute lymphoblastic leukemia) or T-cell lymphoma (cutaneous or peripheral) in at least a partial remission requiring an allo-SCT, <70 years of age, with a matched sibling/unrelated donor. The primary objective was to determine the recommended phase 2 dose (RP2D) of rom from 3 dose levels (1, 2, 3 mg/m2) when combined with BuFlu (AUC 20000 or 16000, Figure). Patients received standard tacrolimus/methotrexate GVHD prophylaxis with ATG for MUDs. Once RP2D was determined, an expansion cohort of up to 30 patients (total) was included. M-rom was initiated between day +28 and +100 for 1 year (2 years max). The effect of rom on NK-cell cytotoxicity was assessed on samples taken pre-transplant, and 1, 3, 6, 12 months post allo-SCT. NK cytotoxicity was assessed by isolating mononuclear cells from patient samples and targeting them against K562 and T-cell lymphoma targets using the calcein-AM assay. Fine-Gray models were used to estimate PFS, OS, and cumulative incidence, and compare survival curves across groups.
Results:
21 patients have been enrolled (Table). One DLT was observed (VOD), at dose level 2, and the RP2D of rom in conditioning was determined to be 2 mg/m2. With a median follow-up time of 10.1 months, the median OS has not been reached (3.3-NR months), with a 1 and 3-year OS probability of 62.8% & 55.8%. The median PFS is 28.2 months (3.8-28.1), with 1 and 3 year PFS of 57% & 30.4%. Cumulative incidence (CI) of NRM at day 100 and 1 year were 14.8% and 20%. CI of grade II-IV aGHVD and extensive cGVHD were 47.6% and 18.5%. The CI of relapse (CIR) was 22.8% at 1 year (95% CI 6.6-44.9%). There was no difference between PFS among patients with MRD versus those without MRD prior to transplant (p=0.96), and no difference in 1-year CIR (p=0.9). PFS and CIR at 1 year was substantially better in the lymphoma than leukemia patients (85.7% vs 44%, p=0.049), and (0% vs 32.1%, p=0.05). No patients with PTCL relapsed, and 3/5 patients with T-PLL are alive, disease free.
13/21 (62%) of patients received m-rom with a median number of 10 cycles (range 1-41). (Table) 7 patients experienced grade 3/4 adverse events (AE), though no patients discontinued m-rom due to toxicity. NK-cytotoxicity was higher at each time point in patients who received m-rom compared to those who did not, though there were insufficient patients to reach statistical significance. When NK-cytotoxicity was assessed between the two groups after starting maintenance, NK-cytotoxicity in the m-rom group was significantly higher than in those without m-rom (p=0.05) (Figure).
Conclusions:
BuFluRom with m-rom is effective at decreasing relapse in patients with T-cell malignancies, with 1-year CI relapse below expected relapse rates for this set of diseases. Toxicities were similar to standard BuFlu alone and the RP2D of rom in conditioning was established at 2 m g/m2. Intriguingly, BuFluRom mitigated the poor outcomes of patients with MRD prior to transplant. Further, early data suggests m-rom enhances NK-cell cytotoxicity post allo-SCT, potentially augmenting the GVL effect and accounting for decreased relapse rates. Long-term follow-up is needed to evaluate these results, but these results suggest the BuFluRom regimen with m-rom could become a new option for patients receiving allo-SCT for T-cell malignancies to mitigate relapse.
Hosing: Nkarta Therapeutics: Membership on an entity's Board of Directors or advisory committees. Popat: Bayer: Research Funding; Abbvie: Research Funding; Novartis: Research Funding; Incyte: Research Funding. Vasu: Boehringer Ingelheim: Other: Travel support; Seattle Genetics: Other: travel support; Kiadis, Inc.: Research Funding; Omeros, Inc.: Membership on an entity's Board of Directors or advisory committees. de Lima: Miltenyi Biotec: Research Funding; Incyte: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees. William: Dova Pharmaceuticals: Research Funding; Incyte: Research Funding; Kyowa Kirin: Consultancy; Merck: Research Funding; Guidepoint Global: Consultancy. Lee: Kiadis Pharma: Divested equity in a private or publicly-traded company in the past 24 months, Honoraria, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties, Research Funding; Courier Therapeutics: Current holder of individual stocks in a privately-held company. Brammer: Kymera Therapeutics: Consultancy; Celgene: Research Funding; Seattle Genetics: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal